Contents
- 1 What Causes Bipolar Disorder |Genetic and Environmental Factors Explained
- 2 Introduction
- 3 Bipolar Disorder as a Multi Factor Condition
- 4 Genetic Causes of Bipolar Disorder
- 5 Neurobiological Causes of Bipolar Disorder
- 6 Environmental Causes of Bipolar Disorder
- 7 Lifestyle Triggers and Daily Influence
- 8 How Genetic and Environmental Factors Interact
- 9 Early Warning Signs That Causes Are Turning Into Symptoms
- 10 How Professionals Diagnose Contributing Causes
- 11 Managing Bipolar Disorder After Understanding the Causes
- 12 Conclusion and Final Thoughts
- 13 Frequently Asked Questions About What Causes Bipolar Disorder
- 14 People Also Ask:
- 15 Important References
- 16 Related Mental Health Blogger Articles | Top Published Posts
What Causes Bipolar Disorder |Genetic and Environmental Factors Explained
Introduction
Learn what causes bipolar disorder in this complete guide. Explore genetic causes, family history, brain chemistry, trauma, environmental triggers, stress, sleep changes, and lifestyle factors that influence bipolar symptoms and long term mental health stability.
Bipolar disorder affects millions of people around the world. Yet many people still wonder what really causes it. Some believe it is only genetic. Others believe it comes from stress, trauma, or major life events. The truth is more complex and far more human.
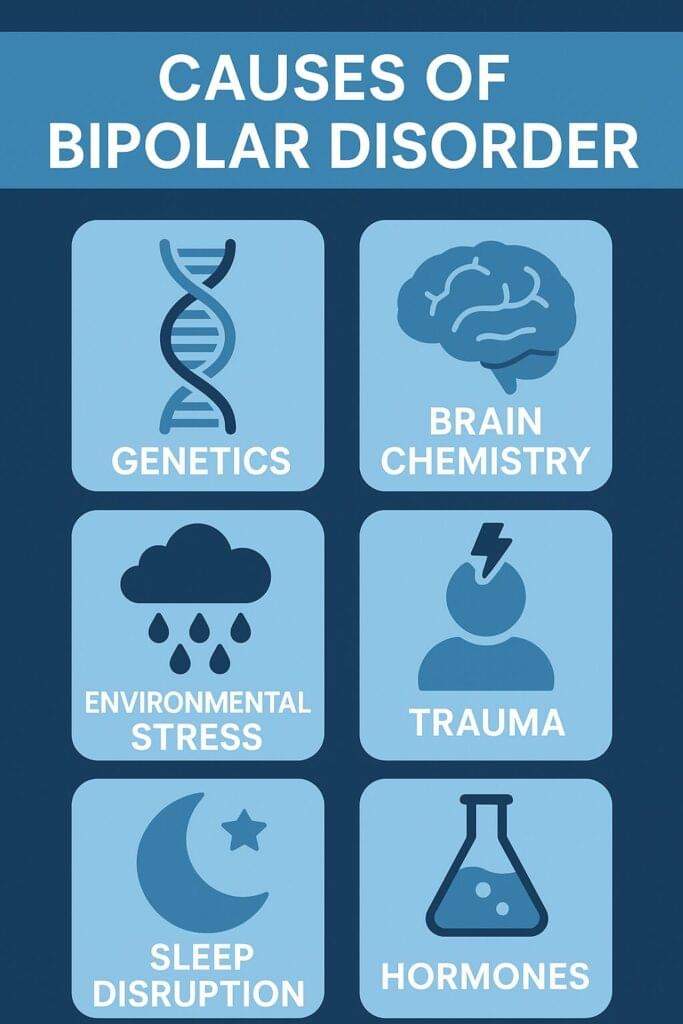
Bipolar disorder develops because of a combination of genetic risks, family history, brain chemistry differences, environmental influences, trauma, lifestyle triggers, and internal vulnerabilities that build over time.
No single cause alone explains it. Instead, several systems interact in a way that slowly shapes how the brain regulates mood, energy, sleep, and emotional responses.
Understanding these causes matters. This helps people recognize early symptoms and It reduces the stigma that often follows a bipolar diagnosis. It gives individuals and families more clarity about why patterns appear the way they do.
It also empowers people to get help early, because early support often leads to better outcomes. This guide walks through every known cause of bipolar disorder in a clear and compassionate way.
You will learn how genetics shape vulnerability, how environmental stress influences the brain, and how daily life triggers can activate symptoms.
This cornerstone article gives you a full picture that blends science, research, and real life experience into one easy to understand resource.
Bipolar Disorder as a Multi Factor Condition
Bipolar disorder is not caused by one singular issue. Instead, several systems inside the body and mind work together in a way that raises or lowers risk. You may have a genetic predisposition that makes you more sensitive to stress or sleep changes or you may come from a family where several people have mood disorders.
If you experienced early trauma, this could shape your emotional development. You may also live in an environment where stress, conflict, or major changes happen often. All of these factors combine and influence the brain over time.
Scientists understand bipolar disorder by studying identical twins, brain imaging scans, genetic patterns, hormone systems, and long term mood tracking data. The research is clear. Bipolar disorder develops through interaction.
People with high genetic risk may never show symptoms if protective factors are strong. People with low genetic risk may develop bipolar disorder if they experience multiple environmental triggers. This interaction makes bipolar disorder a complex and deeply personal condition.
Genetic Causes of Bipolar Disorder
Genetics play one of the strongest roles in the development of bipolar disorder. Studies show that up to 85 percent of the risk is connected to inherited biological traits. This does not mean genes cause bipolar disorder alone.
It simply means the blueprint for mood regulation often begins with inherited patterns. These patterns influence how the brain processes chemicals, responds to stress, and manages emotional changes.
Bipolar Disorder: Mania and Depression Video
Family History and Inheritance
Family history is one of the most reliable predictors. Many people who develop bipolar disorder have a close relative with bipolar disorder, major depression, anxiety disorders, or related mood conditions.
First degree relatives have a significantly higher chance of experiencing symptoms themselves. Children with one bipolar parent have a higher risk. If both parents have bipolar disorder, the risk increases even more.
However, family history does not guarantee someone will develop bipolar disorder. Some relatives may inherit the genes but never develop symptoms because their environment is supportive and stable. Others may develop symptoms only after stressful or traumatic life events.
Twin Studies and Heritability
Identical twin studies offer powerful insight. Identical twins share the same DNA. When one identical twin develops bipolar disorder, the other twin has a much higher chance of developing it as well.
However, identical twins do not always share the diagnosis. This shows that genes are very important but not the only factor. Environment and stress also matter.
These studies help researchers estimate heritability. Bipolar disorder is one of the most heritable mental health conditions, which means genes influence risk more strongly than many other disorders.
Specific Genes Linked to Bipolar Disorder
Scientists continue to identify gene variations that influence mood regulation. These genes affect emotional balance, stress responses, neurotransmitter levels, sleep cycles, and brain development.
Below is a list of known genes and pathways associated with bipolar disorder. Each one contributes to risk in a different way.
Key Genetic Factors
- CACNA1C, which influences calcium channels in brain cells and affects mood stability
- ANK3, which supports nerve signaling
- ODZ4, which influences neural development
- TRANK1, which supports neural growth
- NCAN, associated with structural brain differences
- SLC6A4, a serotonin transporter gene that affects mood
- CLOCK, which influences circadian rhythm and sleep
- BDNF, which supports brain cell growth and emotional regulation
- GSK3B, which affects mood patterns and is targeted by lithium
- DGKH, which regulates intracellular signaling
- NRG1, which affects neural connectivity
- COMT, which regulates dopamine breakdown
- MAOA and MAOB, which influence neurotransmitter metabolism
- Mitochondrial gene variations that affect cellular energy
Each of these genes influences how the brain handles emotional information. Many of these genes also appear in research about depression, anxiety, ADHD, and schizophrenia. This explains why mood disorders often run together within families.
Neurobiological Causes of Bipolar Disorder
Genetics set the foundation. Neurobiology builds the structure. Researchers have found several differences in the brains of people with bipolar disorder. These differences are not flaws. They reflect natural variations in how the brain functions under stress and emotional change.
Brain Structure Differences
Brain imaging studies have found slight differences in areas involved in emotion and decision making. These areas include the amygdala, hippocampus, and prefrontal cortex.
The amygdala helps regulate emotional intensity. The hippocampus helps with long term memory and emotional learning. The prefrontal cortex manages decision making, impulse control, and planning.
These areas may be larger or smaller or may activate more strongly during emotional experiences. White matter patterns may also differ. These variations can influence how the brain moves information from one region to another.
Neurotransmitter Imbalances
Chemical messengers inside the brain play a major role in bipolar disorder. When these chemicals shift quickly or stay imbalanced for long periods, mood swings can occur.
Common Neurotransmitters Involved
- Dopamine, which influences motivation and reward
- Serotonin, which affects mood and emotional balance
- Norepinephrine, which affects energy and alertness
- Glutamate, which supports excitatory signals
- GABA, which supports calm and stability
When these chemicals change too fast or too intensely, the brain may experience mania or depression. Many bipolar medications target these neurotransmitters because they help stabilize the brain’s mood system.
Circadian Rhythm Disruptions
Circadian rhythms control the sleep wake cycle. People with bipolar disorder often experience rhythm disruptions even before symptoms begin.
A small change in sleep timing can trigger mania or depression. Sleep deprivation is one of the most common triggers of manic episodes. Genetic variations in circadian rhythm genes also increase the risk.
Hormonal and Endocrine System Differences
The endocrine system influences stress, energy, and emotional reactions. People with bipolar disorder often show differences in:
- Thyroid hormone levels
- Cortisol stress hormone levels
- Sex hormone shifts
- HPA axis regulation
These systems respond strongly to stress and trauma and can influence mood stability over time.
The Roles of Environmental and Genetics With Bipolar Disorder
Environmental Causes of Bipolar Disorder
Environmental causes do not create bipolar disorder alone. They interact with genetic vulnerability. When stress, trauma, or major life changes occur in someone already genetically sensitive, symptoms can appear or intensify.
Childhood Trauma and Adverse Experiences
Many adults with bipolar disorder report traumatic or difficult childhood events. These experiences can shape how the brain learns emotional survival. Trauma increases stress sensitivity. It weakens emotional regulation. It influences the HPA axis, which controls the body’s stress response.
Common Early Life Risk Factors
- Emotional abuse
- Physical abuse
- Sexual abuse
- Neglect
- Household conflict
- Parent with substance misuse
- Parent with mental illness
- Long term instability
- Chronic bullying
- Poverty or unsafe living environments
These experiences do not guarantee bipolar disorder. They simply raise the risk by changing how the brain responds to stress later in life.
Major Life Stress and Chronic Stressors
Stress plays a big role in activating bipolar symptoms. When stress is constant, overwhelming, or deeply emotional, it can push the brain toward mood instability.
Common Stress Triggers
- Breakups or divorce
- Job loss or career pressure
- Academic stress
- Financial struggles
- Medical problems
- Death of a loved one
- Long term caregiving
- Military trauma
- Moving to a new place
- Major life transitions
Stress does not cause bipolar disorder alone. It activates genetic vulnerability. Stress levels are often the tipping point between stability and symptoms.
Substance Use and Mood Instability
Substance use can worsen bipolar symptoms or trigger the first manic episode. Drugs and alcohol change neurotransmitter levels. They interfere with sleep. They increase impulsivity. They also worsen emotional swings.
Substances That Increase Symptoms
- Alcohol
- Cannabis
- Stimulants
- Opioids
- Hallucinogens
- Synthetic drugs
Some people use substances to cope with mood symptoms. However, this usually creates a cycle that leads to more severe episodes and stronger symptoms.
Sleep Disruption and Irregular Sleep Patterns
Sleep plays an essential role in mood stability. Sleep disturbances often appear before manic or depressive episodes. Even a single night of reduced sleep can trigger mania for someone with bipolar disorder. Consistent sleep routines are one of the strongest protective factors.
Seasonal Patterns and Light Exposure
Many people with bipolar disorder experience seasonal changes in mood. Some feel more manic during spring and summer. Others feel more depressed during fall and winter due to reduced sunlight. Light exposure influences circadian rhythms and melatonin production.
Medical Conditions and Physical Health
Certain medical conditions can increase bipolar risk or trigger symptoms.
H4: Medical Risk Factors
- Thyroid disorders
- Traumatic brain injuries
- Nutrient deficiencies
- Chronic inflammation
- Autoimmune conditions
These conditions place stress on the body and influence hormone balance, which can affect mood regulation.
Social Environment and Relationship Dynamics
Healthy social support protects mental health. Unhealthy dynamics increase stress and emotional strain. Many people experience mood instability when they live in environments where conflict, criticism, or instability are common.
Lifestyle Triggers and Daily Influence
Small daily habits play a major role in mood stability. These triggers often interact with genetic sensitivity and environmental stress.
Irregular Routines
People with unstable routines often experience more mood swings. A consistent daily schedule supports circadian rhythms and emotional regulation.
Unhealthy Nutrition
Food influences energy and emotional balance. High sugar diets, excessive caffeine, alcohol, or nutrient poor meals raise the risk of mood swings.
Low Physical Activity
Movement improves mood stability. Sedentary habits increase depressive symptoms and lower emotional resilience.
High Stress Jobs and Intense Careers
Jobs with long hours, night shifts, or intense pressure often worsen symptoms. People with bipolar disorder thrive with predictable schedules and work life balance.
How Genetic and Environmental Factors Interact
Bipolar disorder develops through interaction. Genes create the foundation. Environment shapes the experience. Daily life triggers activate the system.
The Stress Vulnerability Model
People with a genetic predisposition may remain stable until a major environmental stressor appears. Stress opens the doorway for symptoms to emerge.
Epigenetics and Gene Activation
Trauma and stress can influence how genes express themselves. Environmental events can activate or deactivate certain genetic pathways. This explains why two people with the same genetic risk may have very different life experiences.
Protective Factors
Not everyone with genetic risk develops bipolar disorder. Many protective factors reduce the likelihood of symptoms.
Protective Factors
- Supportive family relationships
- Stable sleep routines
- Healthy lifestyle habits
- Early mental health care
- Stress management skills
- Safe childhood environments
These positive influences help manage genetic sensitivity.
Early Warning Signs That Causes Are Turning Into Symptoms
Many people experience early signals before a full mood episode. Recognizing these signs early can prevent severe symptoms.
Early Signs of Mania
- Increased energy
- Quick speech
- Racing thoughts
- Less need for sleep
- Irritability
- Impulsive spending
- Feeling unusually confident
Early Signs of Depression
- Low energy
- Sadness
- Loss of interest
- Brain fog
- Withdrawing from others
- Changes in sleep
- Feelings of hopelessness
These signs appear before full episodes. Early intervention helps reduce severity and improve long term outcomes.
How Professionals Diagnose Contributing Causes
Mental health professionals do not diagnose bipolar disorder based on mood alone. They look deeply into causes, patterns, and influences.
What the Diagnostic Process Includes
- Evaluation of family history
- Screening for trauma
- Medical testing
- Sleep pattern analysis
- Substance use screening
- Long term mood tracking
- Clinical interviews
This structured approach helps create an accurate diagnosis and a personalized treatment plan.
Managing Bipolar Disorder After Understanding the Causes
When the root causes become clear, treatment becomes more effective. Management involves several layers.
Medication Support
Medications help stabilize mood, balance chemicals, and reduce cycling. They target neurotransmitter systems and regulate energy levels.
Therapy and Emotional Support
Therapies like CBT, DBT, trauma therapy, and sleep therapy help individuals understand patterns and manage stress more effectively. Family support and communication training also help create stability.
Lifestyle Changes That Support Stability
- Regular sleep routines
- Healthy diet
- Consistent exercise
- Stress reduction
- Mindfulness
- Daily structure
- Avoiding alcohol and drugs
- Tracking mood patterns
These habits strengthen emotional resilience and reduce triggers.
Conclusion and Final Thoughts
Bipolar disorder is not caused by one issue. It develops from a complex interaction of genetics, environment, brain chemistry, stress, trauma, and life experiences.
The combination of these factors shapes how mood cycles appear in each person. Understanding these causes helps remove shame and stigma.
It helps people see that bipolar disorder is not a personal failure. It is a medical condition influenced by many forces that interact over time.
When people understand their causes and triggers, they can create better plans for support and stability.
Strong routines, supportive relationships, early treatment, and healthy lifestyle choices can help individuals live full and meaningful lives.
Knowledge brings clarity. Clarity brings strength. Strength builds long term stability.
This complete guide gives you the tools to understand the deeper layers of bipolar disorder and the many factors that shape it. Thank you for reading. Read more below for even more information and resources.
Frequently Asked Questions About What Causes Bipolar Disorder
What actually causes bipolar disorder?
Bipolar disorder develops from a combination of genetic factors, family history, brain chemistry differences, hormonal changes, trauma, chronic stress, and environmental triggers. There is no single cause. The condition forms when biological vulnerabilities interact with life experiences over time.
Is bipolar disorder genetic or environmental?
Bipolar disorder is both genetic and environmental. Genetics account for a large part of the risk. Environment shapes how and when symptoms appear. Most people experience a mix of inherited sensitivity and external triggers.
Can stress cause bipolar disorder?
Stress does not create bipolar disorder alone. However, high stress levels can activate symptoms in someone with genetic risk. Stressful events also increase the intensity of mood swings and can trigger manic or depressive episodes.
Does childhood trauma increase the risk of bipolar disorder?
Yes. Childhood trauma is a major environmental risk factor. Experiences such as abuse, neglect, bullying, and early instability affect emotional development and increase stress sensitivity. These changes make the brain more vulnerable to bipolar symptoms later in life.
Can you develop bipolar disorder without a family history?
Yes. Some people develop bipolar disorder even without family history. This can happen when strong environmental triggers, trauma, or medical conditions interact with smaller genetic risks. Family history raises the risk, but it is not required.
What genes are linked to bipolar disorder?
Research points to genes that influence mood regulation, neurotransmitters, and circadian rhythms. Examples include CACNA1C, ANK3, CLOCK, BDNF, COMT, and several serotonin and dopamine pathway genes. These genes create vulnerability but do not guarantee symptoms.
Can sleep problems cause bipolar episodes?
Yes. Irregular sleep or reduced sleep can trigger manic or depressive episodes. Sleep changes affect the circadian rhythm and stress systems. Many people with bipolar disorder experience symptoms after even one night of poor sleep.
Can drug or alcohol use trigger bipolar disorder?
Drug and alcohol use can trigger bipolar symptoms in someone who already has the underlying vulnerability. Substance use disrupts brain chemicals, increases impulsive behavior, and interferes with sleep, all of which raise the risk of mood episodes.
Do hormones play a role in bipolar disorder?
Yes. Hormone changes influence mood and energy. Thyroid problems, cortisol stress hormone changes, and reproductive hormone shifts can increase symptoms. Many people experience episodes during hormonal transitions such as postpartum or perimenopause.
Are people born with bipolar disorder?
People are not born with visible symptoms. However, they may be born with genetic traits that increase the risk. Symptoms often appear during late teens or early adulthood when genetics and environment interact.
What environmental triggers can worsen bipolar disorder?
Common triggers include stress, trauma, sleep disruption, substance use, major life changes, relationship conflict, high pressure jobs, seasonal changes, physical illness, and unstable routines. These factors activate symptoms in someone with genetic sensitivity.
Can bipolar disorder develop after a major life event?
Yes. Major life events like a breakup, job loss, trauma, or sudden stress can trigger the first manic or depressive episode. These events place pressure on the emotional system and can reveal underlying vulnerability.
Can brain chemistry cause bipolar disorder?
Brain chemistry plays a major role. Differences in dopamine, serotonin, norepinephrine, glutamate, and GABA affect mood stability. When these chemicals shift quickly or stay imbalanced, they can lead to manic or depressive episodes.
Does bipolar disorder run in families?
Yes. Bipolar disorder often runs in families. About half of people diagnosed have a close relative with bipolar disorder or another mood disorder. Family history is one of the strongest predictors of risk.
Can a medical condition cause bipolar symptoms?
Yes. Thyroid problems, traumatic brain injuries, chronic inflammation, nutrient deficiencies, and certain neurological issues can contribute to mood instability. These conditions may trigger symptoms or intensify existing bipolar patterns.
How do genetics and environment interact in bipolar disorder?
Genes create the foundation for vulnerability. Environment activates or suppresses that vulnerability. When stress, trauma, or sleep disruption interacts with genetic sensitivity, symptoms can develop or worsen. This interaction explains why experiences vary from person to person.
Can bipolar disorder be prevented?
Bipolar disorder cannot always be prevented. However, stable sleep routines, stress reduction, early mental health care, trauma support, and healthy lifestyle habits can reduce the risk of severe episodes and help delay symptom onset.
What are early signs that causes are becoming symptoms?
Common early signs include increased energy, irritability, fast thoughts, reduced sleep, sadness, brain fog, withdrawal, and changes in daily habits. These signals often appear before a full manic or depressive episode.
Can someone have bipolar disorder without realizing it?
Yes. Many people live with symptoms for years before receiving a diagnosis. Changes in mood may feel normal or may be misunderstood as stress, personality traits, or emotional reactions.
When should someone seek help for suspected bipolar disorder?
A person should seek help when mood changes interfere with daily life, cause distress, affect relationships, disrupt work or school, or create sudden changes in sleep, energy, or behavior. Early help improves long term outcomes.
People Also Ask:
What is the root cause of bipolar disorder?
There is no single root cause. Bipolar disorder develops through a combination of genetic risk, family history, brain chemistry differences, trauma, stress, and environmental triggers that influence mood regulation over time.
Can bipolar disorder be triggered later in life?
Yes. Bipolar disorder can appear in adulthood when stressful events, medical issues, or sleep disruption interact with an underlying genetic vulnerability. Late onset bipolar disorder is less common but still possible.
What age does bipolar disorder usually start?
Bipolar disorder often begins in late teens or early adulthood. Some people notice symptoms during childhood, while others experience their first episode later in life after a major stressor or hormonal change.
Can trauma cause bipolar disorder?
Trauma does not create bipolar disorder alone. However, trauma increases vulnerability by changing how the brain processes stress and emotions. This makes symptoms more likely in someone with a genetic predisposition.
What environmental factors contribute to bipolar disorder?
Environmental risk factors include chronic stress, childhood adversity, relationship conflict, substance use, irregular sleep, high pressure jobs, major life events, medical illnesses, and seasonal changes.
Does bipolar disorder run in families?
Yes. Bipolar disorder often appears in families due to strong genetic influence. A person with a close relative who has bipolar disorder has a higher chance of developing symptoms.
Can bipolar disorder be caused by hormonal changes?
Yes. Hormonal changes can influence mood and energy. Thyroid problems, cortisol imbalances, postpartum changes, and reproductive hormone shifts can contribute to bipolar symptoms or worsen mood episodes.
Can lack of sleep cause bipolar episodes?
Yes. Lack of sleep is one of the strongest episode triggers. Even one night of sleep loss can lead to mania or hypomania in someone with bipolar disorder. Stable sleep routines protect mood stability.
What medical conditions mimic bipolar disorder?
Conditions like thyroid disorders, ADHD, major depression, borderline personality disorder, PTSD, and some neurological conditions can mimic or overlap with bipolar symptoms. A full evaluation is needed for accuracy.
Can bipolar disorder go away on its own?
No. Bipolar disorder does not disappear without treatment. However, symptoms can improve with proper care, medication, therapy, lifestyle changes, stress reduction, and early intervention.
Important References
1. National Institute of Mental Health (NIMH)
https://www.nimh.nih.gov/health/topics/bipolar-disorder
NIMH is one of the most authoritative sources for psychiatric research. It offers detailed information about bipolar disorder, including causes, symptoms, genetics, brain research, and treatment options.
2. Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/bipolar-disorder
Mayo Clinic provides medically reviewed content about bipolar disorder. Their guides cover causes, risk factors, diagnosis, complications, brain chemistry, and long term management strategies.
3. Cleveland Clinic
https://my.clevelandclinic.org/health/diseases/9294-bipolar-disorder
Cleveland Clinic delivers expert backed information on bipolar disorder, including genetic risks, environmental factors, triggers, symptom patterns, and treatment approaches.
Related Mental Health Blogger Articles | Top Published Posts
1. How Social Media Affects Teen Mental Health: A Comprehensive Guide
This post explores how digital connection, social platforms, and constant online engagement shape teenage mental health. It breaks down how social media influences self-esteem, anxiety, depression, body image, sleep, and social comparison. The guide also offers advice for teens, parents, and caregivers on how to maintain a healthier digital balance and protect emotional well-being in the online age.
2. When Is Mental Health Awareness Month? Dates, Themes, and Participation Ideas
This article outlines the history and purpose of Mental Health Awareness Month, explaining when it occurs, why it matters, and what each year’s theme represents. It gives readers practical ideas for participation — from raising awareness to organizing community events, sharing resources, and promoting mental wellness. The post also encourages early intervention, community support, and advocacy for better mental health access worldwide.
3. What Are the 10 Most Common Types of Mental Illness? A Beginner’s Guide with Examples
In this beginner-friendly article, Mental Health Blogger offers an overview of the ten most common mental illnesses. It lists each condition, describes symptoms, and gives real-world examples to help readers understand how mental health can present in different ways. The guide aims to educate readers on the variety and prevalence of mental health disorders, reduce stigma, and encourage understanding and compassion.
Thank you very much for reading. You can find more mental health related articles on our homepage Mental Health Blogger



